We give the best Services
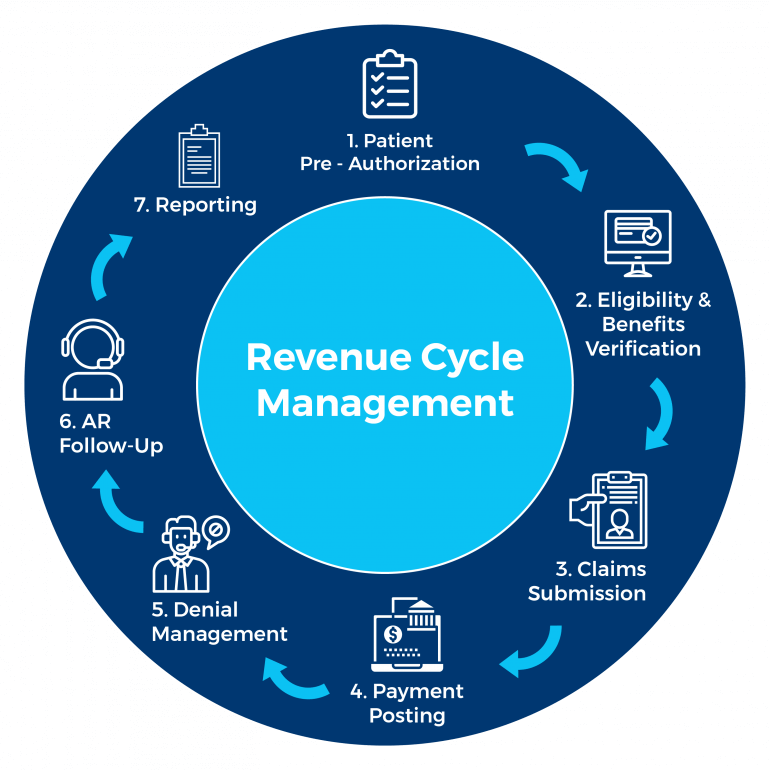
Handling medical claim denials is one of the most time-consuming yet essential aspects of successful revenue cycle management. Unresolved denials can lead to significant revenue loss, impacting the financial health of healthcare providers. At Statmed RCM Solutions, we take a systematic, hands-on approach to managing denied claims, ensuring maximum recovery of lost revenue.
Our process begins with thorough claim analysis, identifying the root cause of the denial and determining the best course of action. Next, we prioritize claims based on patient demographics and business rules, focusing on cases that offer the highest reimbursement potential. Our experts then implement proactive measures to reduce future denials by improving billing accuracy and compliance.
Our goal is to maximize reimbursements for denied and underpaid claims. Through our structured appeal process, we aggressively pursue payments from contracted payers, ensuring that every claim receives the attention it deserves.
What You Can Expect from Our Denial Management Services:
With Statmed RCM Solutions, you can rest assured that every denied claim is thoroughly reviewed and recovered, leading to greater financial stability and optimized revenue cycles.
Contact
- Lakshmi arcade, 3rd main, next to ring road , shanthinagar , hassan 573201 KA
- +1 216-369-8653
